While the concept behind trauma-informed care is simple—trauma-informed care is respectful care—the practical work of making it a reality in clinical settings requires an intentional approach. It’s important to note that trauma-informed care does NOT require health care providers to ask for disclosures of trauma nor to be experts in treating trauma symptoms. Instead, trauma-informed principles and concepts can be applied during all clinical interactions to establish trust and help patients feel in control. Given that many adults in the U.S. have experienced some type of traumatic event, it’s crucial health care providers adopt a trauma-informed approach.
What does respectful care look like for those who have experienced trauma? What do we do and say to ensure we’re doing it “right”? How do we ensure we don’t retraumatize our patients? While these questions can be a challenge to address, asking and answering these them can lead us to better health care experiences and outcomes for all patients.
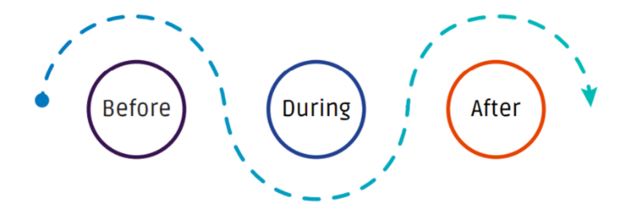
If you’ve recently found yourself asking the questions posed above, you’re not alone. Given all the buzz around trauma-informed care in the past few years, many providers know this care is important. However, many providers haven’t received practical, step-by-step guidance on how to provide it. The National Coalition for Sexual Health and the Clinical Training Center for Sexual and Reproductive Health partnered to craft a practical solution. Together, we created a roadmap for clinicians seeking to provide trauma-informed physical examinations, with an emphasis on pelvic exams. The Clinician Guide for Trauma-Informed Care is a practical tool with action steps and scripts for all three phases (before, during, and after) a clinical visit. While focused on pelvic exams, this tool includes universal principles and sample language that are applicable to any health care service.
Key takeaways in each phase of the exam
First, before the exam, providers need to consider:
– the physical environment (temperature, natural light, multiple options for seating);
– offering a support person (2020 ACOG guidance also recommends a chaperone be present for all breast, genital, and rectal exams);
– establishing rapport before the patient undresses;
– discussing patient goals and process of the exam;
– and assuring them they are in control—they can stop or pause at any time.
During the exam:
- explain the steps and describe what you are going to do and why;
- ask questions and gain permission at every step of the procedure and check in often;
- be mindful of re-traumatizing or offensive words and phrasing such as “relax” or “open wide;”
- and watch for signs of discomfort and distress.
Last, after the exam:
- allow the patient to dress before finishing the appointment;
- discuss and recap the visit in simple and clear language;
- make an action plan for a follow-up;
- provide referrals and helpful resources;
- and confirm their documentation preferences.
What if someone does disclose past and/or current trauma?
First and foremost, offer validation, empathy, and acknowledgment of the disclosure. For example, “Thank you for trusting me with your story. I really appreciate the courage it took to share that with me.” You can also confirm confidentiality and let the patient know they can say as little or as much as they’d like to. You may want to ask about the patients’ wellbeing in their daily life as well as if the disclosure impacts their visit and how they might want the information documented. For instance: “Given what you’ve just shared with me, is there anything I can do to make you feel more comfortable today?
There are also a few things not to do: do not multi-task, minimize their trauma, show pity, or tell them they need to get help. Instead, offer a list of resources so that they may get the support they deserve.
Bottom Line
The good news is that you don’t need to memorize these steps with a mnemonic device: This tool is free, online, easy to print, and includes a self-assessment to identify ways to help make your clinical exams more trauma-informed. Try it out and then let us know how it worked for you and your patients. We hope this guide can help you and your clients at every visit and in many contexts.




