Understanding if, when, and under what circumstances someone wants to become pregnant is a key part of high-quality reproductive health for all people. For people with rheumatic and musculoskeletal diseases (RMD) including systemic lupus erythematosus (SLE) and psoriatic arthritis, there are additional risks and considerations when thinking about pregnancy desires. Pregnancy itself can worsen some RMDs as well as affecting pregnancy outcomes, like increasing the risk of pregnancy loss, preterm delivery, and growth restriction, and some medications used to treat RMD may be teratogens. So, when talking to people with RMD who are able to become pregnant, asking about pregnancy desires is particularly important. For people with RMD who don’t want to become pregnant right now, there are some key facts that providers need to know to ensure you are offering safe and effective birth control options to meet the needs of your patients with RMD. Lucky for us, we were able to get our questions answered by the experts on birth control and RMD.
What diagnosis are included in RMD?
There are many rheumatic and musculoskeletal diseases and conditions including fibromyalgia, lupus, psoriatic arthritis, rheumatoid arthritis, and scleroderma. For a complete list go to: www.rheumatology.org/I-Am-A/Patient-Caregiver/Diseases-Conditions
What birth control methods can people with RMD safely use?
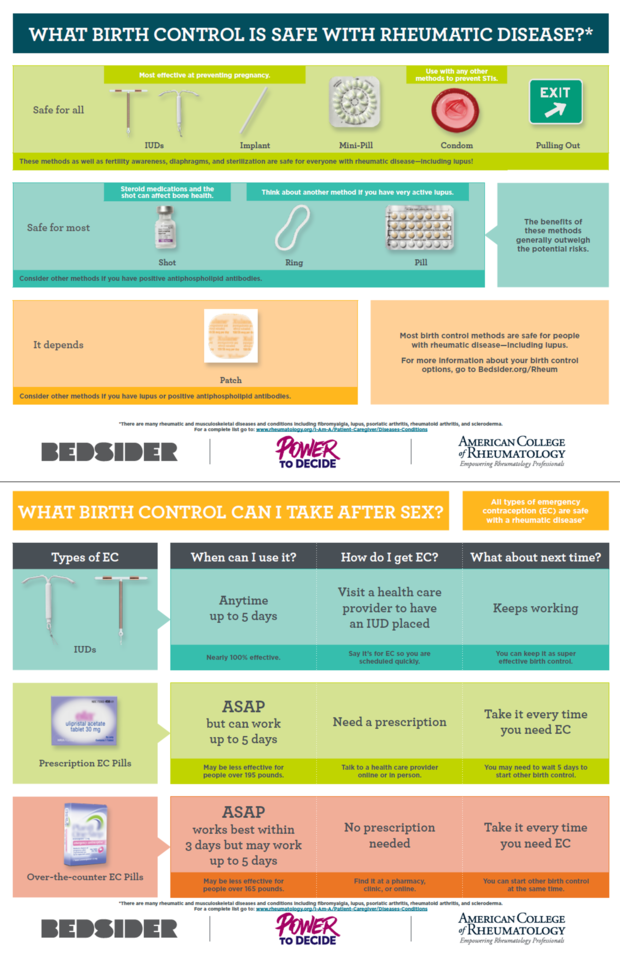
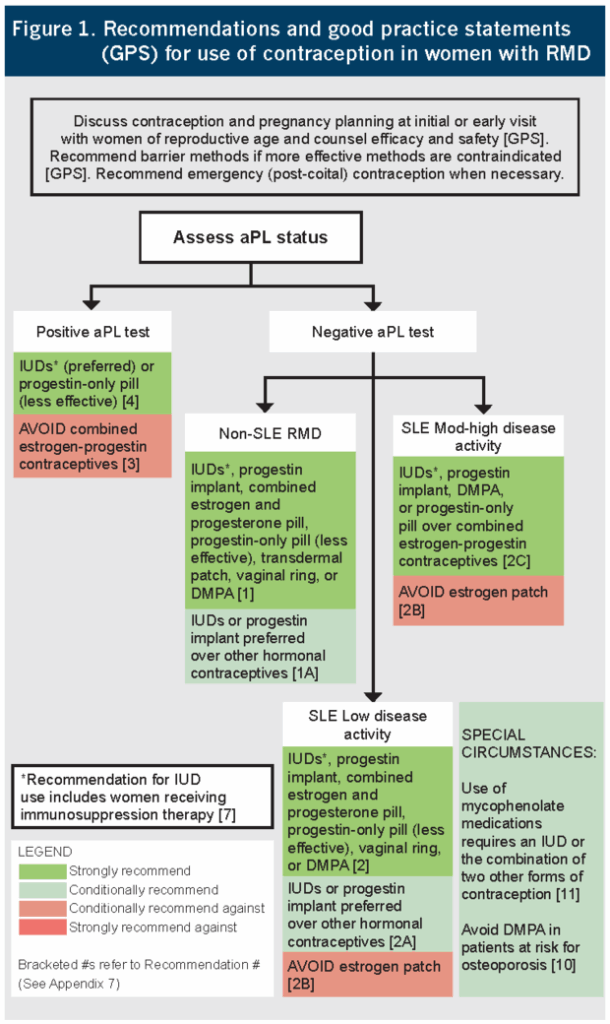
First things first, hormones, including estrogen and progestin in birth control, are not contraindicated for people with RMD and most birth control methods are safe for people with RMDs, including SLE. Anyone with RMD, regardless of diagnosis or disease state, can safely use any type of IUD, the implant, progestin-only pills, behavioral methods, like withdrawal, and barrier methods, like condoms and diaphragms. And there are no restrictions on birth control methods for people who:
- Have tested negative for antiphospholipid antibodies (aPL),
- Don’t have SLE,
- Are not at increased risk of osteoporosis, or
- Are not taking medications containing mycophenolate mofetil or mycophenolic acid.
Because of potential additional risk of venous thromboembolism (VTE), people who have aPL should not use the shot or methods with estrogen, like the pill, patch, or ring. The shot, a.k.a. DMPA, name brand Depo-Provera, should be used with caution. “There is a signal that DMPA is pro-thromboticaless so than estrogen-containing contraception but probably more so than the progestin-only pill. Long story short, DMPA is safe for most people, but we need more data about its safety profile among people with baseline elevated pro-thrombotic risk,” says Mehret Birru Talabi, MD, Assistant Professor of Medicine in the Division of Rheumatology and Clinical Rheumatology at the University of Pittsburgh.
And people with lupus who have a negative aPL test can use the pill and ring but should not use the patch. “The patch gives a higher constant level of estrogen than the combination birth control pills currently on the market and there’s a theoretic concept that estrogen might make active lupus worse, so the guidelines recommend against using the patch for people with thrombotic risk from very active lupus,” say Megan Clowse, MD, MPH.
What about emergency contraception (EC)?
All types of EC are safe for all people with RMD. That means that anyone with RMD can use EC pills, like levonorgestrel (Plan B and generic) or ulipristal acetate (ella), as well as a copper IUD (Paragard) or a 52mg LNG-IUD (Liletta or Mirena) for EC.
Does RMD or its treatment affect any birth control methods?
There are two ways that RMD and its treatments might affect birth control—it could increase the side effects of a particular method, or it could make birth control less effective. For example, people with an underlying risk of osteoporosis because of their RMD or for people who are using medications that use glucocorticoids may wish to consider options other than the shot because of the additional bone health risk—although data have not demonstrated that the bone loss is irreversible.
Additionally, with the medications mycophenolate mofetil and mycophenolic acid, which are used to treat some RMDs, there is a concern that they may decrease the effectiveness of hormonal birth control methods, like the patch, ring, and combination pill. For people who are taking mycophenolate-containing medications, which are teratogens, guidelines recommend either a highly effective methods, like an IUD or implant, or doubling up on methods, sometimes called “dual method use”, such as using both condoms and birth control pills at the same time to increase effectiveness.
Who can offer contraceptive services to patients with RMD?
If you offer birth control to people without RMD, you can discuss, offer, place, and prescribe birth control to people with RMD. That means, primary care providers and OB-GYNs (as well as rheumatologists!) can offer birth control to people with RMD. If you have questions or are unsure about the safety or effectiveness of a birth control method for a patient with RMD, the best resources are the American College of Rheumatology’s guidelines and the CDC’s Medical Eligibility Criteria.
What other resources are available for providers about birth control services for people with RMD?
For providers, the best resources are the 2020 ACR Guideline for the Management of Reproductive Health in Rheumatic and Musculoskeletal Diseases and pocket card, additional reproductive health resources can be found on their website on Reproductive Health and Rheumatic Disease.
For patients, ACR and Bedsider are excited to introduce this two page tear sheet on birth control and EC for people with rheumatic and musculoskeletal diseases. Stay tuned for updates on how to order these free tear sheets and posters for your practice directly from ACR.