People often choose IUDs because they are safe for almost everyone, highly effective at preventing pregnancy, don’t interrupt the moment, and while they do require a health care provider to start using, none of them require ongoing maintenance once they are placed, such as prescription refills or daily dosing. Helping your patients decide between the five IUDs currently available in the US involves weighing their preferences for a hormonal IUD, effects on bleeding patterns, anticipated duration of use, if they need emergency contraception (EC) today, as well as what IUD(s) are available.
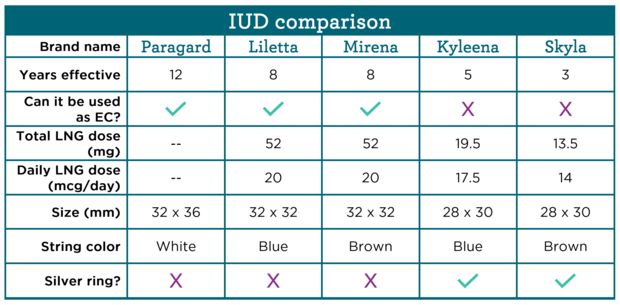
This chart has a side-by-side comparison of IUDs currently available in the US. Providers can use this chart, sample answers to some of the most frequently asked questions from patients, and counseling tips to help patients determine which IUD might be the best fit for them.
How long does an IUD last as birth control?
Sample answer: Three to 12 years depending on the IUD, but you can have it removed anytime for any reason. The non-hormonal, copper IUD (brand name Paragard) is effective for at least 12 years. All of the hormonal IUDs contain the same hormone, levonorgestrel (LNG), and how long they are effective for depends on how much hormone is in the IUD. IUDs with more hormone to start with, such as Mirena and Liletta, are effective for up to eight years, while Skyla which has the lowest dose of hormones to start is only effective for up to three years.
Additional counseling may include that the known duration of effectiveness might be different than the FDA-approved duration of effectiveness, for example, the copper IUD is FDA-approved for 10 years while evidence shows that it continues to be effective for at least 12 years. Some people may want to continue using an IUD up to the evidence-based duration of effectiveness when that is beyond the FDA-approved duration, while others may not—either choice is okay. And in order to provide patient-centered care and respect your patient’s bodily autonomy, any IUD should be removed at any time that a patient requests it for any reason before the maximum duration of effectiveness is met.
Can an IUD be used after unprotected sex?
Sample answer: Yes, placement of a copper IUD (Paragard) or an IUD with 52mg of LNG (Liletta and Mirena) is more than 99% effective as emergency contraception (EC), which means that it prevents pregnancy before it starts.
Either of these three IUDs (Paragard, Liletta, or Mirena) can be placed up to five days after unprotected sex and can be continued without the need for a backup method. The other LNG-containing IUDs (Skyla and Kyleena) have not been studied for use as EC, so we don’t know if they work in that way.
Does the amount of hormones in an IUD change the side effects?
Sample answer: All hormonal IUDs have the same hormone in them, so the most common side effects are similar—irregular, unpredictable vaginal bleeding that usually becomes lighter over time and no bleeding at all for some users. All of the IUDs have very low doses of hormones (significantly lower than other hormone-containing methods), and they don’t have estrogen so there are no estrogen-related side effects, such as breast tenderness.
Additional counseling can include that the more LNG in an IUD, the more likely people are to have amenorrhea, with around 20% of Mirena and Liletta users, 12% of Kyleena users, and 6% of Skyla users having no periods after one year of use. Questions to understand if someone is hoping for menstrual suppression can help determine if an IUD with a higher dose of LNG might be a better fit, while someone who prefers not to have amenorrhea may prefer an IUD with a lower dose of LNG or a non-hormonal, copper IUD which will not affect the timing of menses.
Does the amount of hormones change over time?
Sample answer: Yes. The amount of hormone in each of the hormonal IUDs releases decreases over time, but even as the doses decrease, all the IUDs continue to be highly effective at pregnancy prevention for the entire evidence-based duration of use.
Providers can share information about specific doses and decreasing rates of LNG in each IUD as requested:
- A Liletta IUD contains 52mg of LNG when it is placed, and it is initially released at approximately 20 mcg per day. Over the next six years (the FDA-approved duration of use), the dose decreases to approximately 8.6 mcg/day. If someone uses a Liletta IUD for six years, the average daily dose is 14.3 mcg per day.
- A Mirena IUD contains 52mg of LNG when it is placed, and it is initially released at approximately 20 mcg per day (that’s the same as Liletta). Over the next five years the dose drops to 10 mcg/day and by seven years, the dose decreases to approximately 8 mcg per day.
- A Kyleena IUD contains 19.5mg of LNG when it’s placed, and it is initially released at approximately 17.5 mcg per day. Over the next five years, the dose decreases to 7.4 mcg per day for an average dose of 9 mcg per day over the five years.
- A Skyla IUD contains 13.5 mg of LNG when it’s placed, and it is initially released at approximately 14 mcg per day. Over the next three years, the dose decreases to 5 mcg per day for an average dose of 6 mcg per day over the three years.
Does the size of an IUD matter?
Sample answer: Probably not. IUDs are safe and fit almost anyone with a uterus, which means regardless of how old you are or if you have had a baby before (which can both change the size of the uterus), you can probably use any of the IUDs. Before placing the IUD, the provider will check the size of your uterus to ensure the IUD you’ve selected will fit.
Having sample IUDs in the office that patients can see and touch can help people understand the size differences between different IUDs, which is 4-6mm from the largest to smallest. While almost all patients can use all types of IUDs, someone may prefer a smaller one, and that’s enough reason to offer it.