“Reason for visit: Possible expulsion.” When we hear this, we always hope our patient is mistaken.
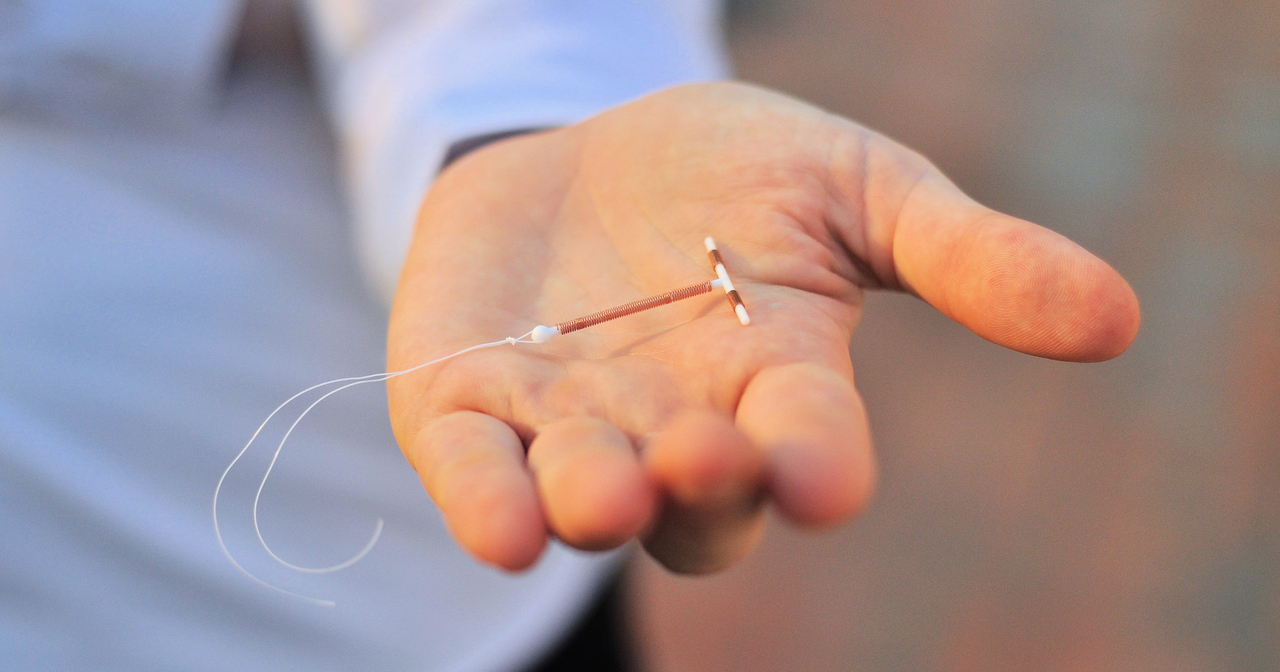
An expulsion is when an intrauterine device (IUD) comes out of the uterus on its own and it happens for about 1 in 20 IUD users. Expulsion leaves the patient vulnerable to unintended pregnancy. A recent study by Madden and colleagues examined this phenomenon and the risk factors associated with it.
What causes an expulsion?
One thought has been that expulsions are due to a small uterus—for example, when the patient is young or has not yet had a baby. Anatomically, this makes sense. If we try to place an IUD inside a uterus that is barely larger than the device, wouldn’t there be a higher chance the uterus will expel it? Despite the importance of this question, it has been hard to answer.
Studying expulsion
The new study focused on IUD users participating in the Contraceptive CHOICE Project. The CHOICE Project was a study of over 9,000 women who received contraceptive counseling, were given the method of their choice at no cost, then were followed for up to 3 years afterwards. For this analysis, every participant with a suspected expulsion had her chart reviewed by two of the investigators. Among the 5,053 women who received an IUD, there were 432 expulsions. This amounts to 6.2 expulsions per 100 IUD users over the course of a year. This is around what we would expect based on previous research.
What did the study find?
The great thing about this study is that it had enough women using IUDs to look at smaller groups of women. This let us explore whether age, parity, or other characteristics of our patients were related to expulsion. The study found that:
- Women under age 20 had a higher rate of expulsion (10.5/100 women per year).
- Among women over age 20, those who were nulliparous had a lower expulsion rate compared to those who had one or more children (3.2 versus 7.2/100, respectively).
- Nulliparous women using the levonorgestrel IUD (Mirena™) had lower expulsion than parous women (3.8 versus 7.9/100).
- Nulliparous women using the copper IUD (ParaGard™) had slightly more expulsions than parous women, although this finding was not statistically significant (6.0 versus 5.5/100).
- Women with self-reported heavier periods at baseline had a higher rate of expulsion overall (8.8/100).
- In a model controlling for women’s characteristics, only being under age 20 and heavy periods were associated with increased risk of expulsion for both types of IUD.
That teens have a higher expulsion rate is not news. But the observation that parity was not associated with expulsion is. This finding could help allay concerns about providing IUDs to nulliparous patients. It’s also important to keep these findings in context. Expulsions happen, but they occur in a minority of patients, even younger patients.
What does this mean for practice?
The largest implication of this study is that parity was not associated with IUD expulsion. Patients who are younger and those with heavy menses at baseline are at a higher risk of expulsion, but overall risk is still low. Everyone deserve access to their preferred method of contraception—regardless of their age, menses, or whether or not they have had children yet.