Recently on vacation while sitting around on the beach chatting, a friend told me about their clinic visit earlier that week: “My doctor said it was time for my Pap, but if I didn’t want a speculum exam, I could swab myself. So I did! It was easy—I just fished the swab around inside, and that was it!”
They shared that they’d never been offered that before and, more importantly, wondered why they hadn’t.
What is HPV self-collection?
Human papillomavirus (HPV) self-swabbing is new around these parts (pun intended). In May 2024, the FDA approved two tests for self-collected vaginal samples, under the brand names Onclarity HPV and Cobas HPV. In February 2025, the American Society for Colposcopy and Cervical Pathology (ASCCP) released the first U.S. guidelines on self-collected HPV screening and how to manage those results. While it’s fresh here, HPV self-collection has already been available for years in Australia and Europe.
But it’s not a Pap; think of it as HPV testing with a new collection route. Cytology still requires cervical cells collected by a provider.
Who can I offer HPV self-collection to?
HPV vaginal self-swabbing can be offered to a lot of people and especially opens up new possibilities for patients who’ve avoided cervical cancer screening because speculum exams feel uncomfortable, painful, or even impossible. This can be common for people with:
- a history of trauma
- gender dysphoria related to their genitals
- vaginal problems like vaginismus or vaginal stenosis
- certain medical conditions or disabilities
- and particular spiritual and cultural practices and beliefs
Who shouldn’t self-swab for cervical cancer screening?
While HPV vaginal self-swabbing is safe and effective, it’s not for everyone. It’s not recommended for:
- people living with HIV
- people whose gestational parent took the medicine diethylstilbestrol (DES) while they were in utero
- and people who need screening under 25 years old
It’s also not recommended for patients who are currently menstruating, have used any kind of vaginal product in the last 48 hours, have any vaginal or pelvic symptoms (bleeding, discharge, pain, etc.) or a history of abnormal paps or HPV.
When should individuals start cervical screening and how often should they test?
Of course there can’t be a single answer! Different organizations have different recommendations on when to start cervical cancer screening, which screening test to use, and routine follow up intervals. For average risk patients:
- American Cancer Society (ACS) recommends starting screening at age 25, with primary high risk HPV testing every 3 years for self-collected swabs and every 5 years for provider-collected samples.
- The US Preventive Services Task Force (USPSTF) recommends starting screening at age 21, with cytology-based screening (Pap testing) every 3 years until age 29. Then, from age 30-65 they recommended either primary high risk HPV testing or Pap with HPV co-testing every 5 years or Pap without hpv testing every 3 years.
Both the American College of Obstetrics and Gynecology (ACOG) and the American Society for Colposcopy and Cervical Pathology (ASCCP) formally endorse the USPSTF and support the ACS recommendations.
So, with patients, deciding about self-collection can be a shared-decision making conversation. Some patients will be stoked to have this option, while others will still prefer clinician-collected samples. And for people who prefer self-collection, it’s reasonable, and evidence-based, to recommend starting at age 25–following the ACS guidelines.
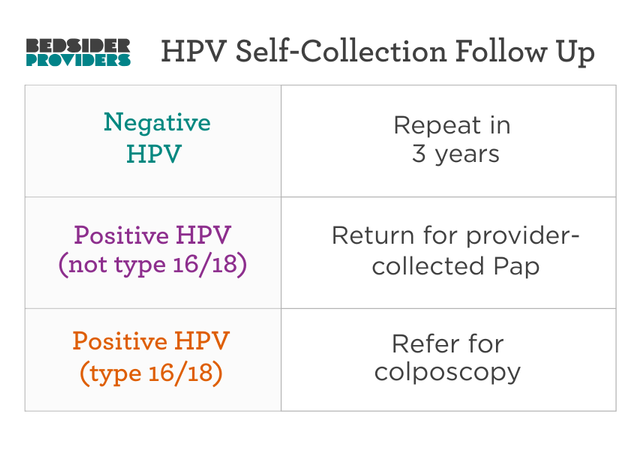
What do I do with HPV self-collection results?
Based on the ASCCP recommendations:
Is HPV self-swabbing as good as provider-collected samples?
Evidence shows self-collected samples are equivalent to clinician-collected in detecting high-risk HPV. HPV is widespread; 80-90% of people will have it at some point in their lifetime and most will clear it within 2 years through our own immune systems. There are over 200 types of HPV, but only a small fraction of those are what are considered to be “high risk” for causing cancer. Together, types 16 and 18 cause about 70% of cervical cancers. Because most cervical cancers occur in people who have not been regularly screened, self-swabbing is an important alternative to the traditional pap smear.
How do I explain to patients how to collect an HPV vaginal sample?
It’s pretty simple:
- Hand the patient one of the approved test swabs.
- Tell them to hold the swab about 3-4 centimeters down (about the length of a pinky finger)
- Have them get in a comfortable position for collection (standing, squatting, or lying down all work)
- Advise them to insert the swab almost all the way to where they are holding it and then rotate the swab 4 times for about 20 seconds, gently touching the sides of the vagina
- Have them remove the swab, put it back into the tube, cap it, and they’re done.
The National Cervical Cancer Coalition has an infographic you can download and share with patients.
Don’t forget about HPV prevention
If your patient is having an HPV freak out with all the alien cell talk, encourage them to take a deep breath and offer to talk about some of the things to prevent HPV:
- get fully vaccinated against HPV
- Cut down/quit/don’t smoke cigarettes (to help prevent persistent HPV infection)
HPV is almost entirely transmitted through skin-to-skin contact, and while consistent barrier use (like condoms) can significantly reduce HPV transmission, it doesn’t cover all touching skin, isn’t possible for all sexual anatomy configurations, and is not always a part of sexy time. Can sex toys transmit HPV? Possibly, but even if so, rarely.
How do I implement HPV self-collection in my practice?
- Check with your lab: Adding self-collection is usually straightforward and just requires having the right swabs on hand, and knowing how to order one of the two tests mentioned above.
- Anticipate questions: Patients may want to know more about this new option before they dive in. Take the time for education and help them decide which cervical cancer screening is right for them.
What about the at-home HPV self-swabs?
For now, there is only an in-clinic option for self-collection that is covered by insurance. But down the road, the test that someone can do at home and then mail to the lab will hopefully be more widely available. At-home HPV testing exists now but only as a cash pay option (and it’s quite expensive); insurances aren’t on board quite yet. If people can, and want to, pay out of pocket, for at home testing it is a safe and effective option for cervical cancer screening for average risk individuals.
Bottom line
HPV self-collection is here. It’s evidence-based, patient-centered, and a new tool to help improve cervical cancer screening. Go forth and help your patients choose their own HPV screening adventure.




